A Basic Overview:How CRO Companies Work

Alexander Doroshenko | Posted on June 19, 2025
Discover how Contract Research Organization (CRO) companies operate, their services from preclinical studies to post-marketing, and key tips for successful pharma-CRO partnerships.
- Introduction
- Typical CRO services
- Why Outsource to CROs
- How CRO Services Support the Drug Development Lifecycle
- Stakeholders and Workflow in a Sponsor–CRO Collaboration
- 2025 Trends in Clinical Trials Outsourcing and CRO Innovation
- Benefits and Challenges of CRO Partnerships
- How to Choose the Right CRO: Key Selection Criteria for Sponsors
- Conclusion
Introduction
Contract Research Organizations (CROs) are companies that provide research and development services to the pharmaceutical, biotechnology, and medical device industries on a contract basis. In essence, a CRO acts as an external drug-development partner, handling various R&D tasks that a sponsor company chooses to outsource. According to international Good Clinical Practice guidelines (ICH), a CRO is defined as “a person or an organization… contracted by the sponsor to perform one or more of a sponsor’s trial-related duties and functions” [1].
Historical context: The CRO industry took shape in response to growing R&D demands. In the early 1980s, pharmaceutical firms that traditionally did all research in-house began facing capacity issues. This led to the formation of the first CROs, which stepped in to provide overflow R&D capacity when internal resources were stretched [2]. Regulators formally recognized this model by the late 1980s – for example, the U.S. FDA added provisions allowing sponsors to transfer trial obligations to independent CROs [3]. Over subsequent decades, pharma and biotech companies increasingly embraced outsourcing to cope with rising development costs and complexity.
The CRO sector grew rapidly and is now a major global industry (approaching $50 billion in annual contract clinical-service spending as of 2022 [4]). Today’s CRO companies offer broad service portfolios spanning early drug discovery, preclinical testing, clinical trial management, data analysis, and regulatory affairs [5].
Note: CROs are distinct from CMOs/CDMOs that focus on drug manufacturing – see our blog post on CMOs and CDMOs for more on those roles.
Typical CRO services
Most CRO services cover the full drug development lifecycle. A sponsor can contract a CRO for laboratory research (e.g. synthesis and preclinical studies like ADME and toxicology), for executing clinical trials (Phase I through IV), for specialized support like regulatory affairs filings or medical writing, or for post-marketing studies and real-world evidence collection. Many CRO companies provide “end-to-end” solutions, meaning they can plan and run an entire clinical program. Others specialize in particular stages or tasks. In practice, sponsors often use multiple CRO partners to leverage niche expertise or regional capabilities [6]. For example, one CRO might handle in-vitro screening and animal toxicology, while another manages the Phase II–III clinical trials. Overall, a CRO’s service portfolio typically includes study protocol design, site selection and site management, patient recruitment, clinical monitoring, data management and biostatistics, pharmacovigilance (drug safety monitoring), regulatory document preparation, and trial logistics coordination [7].
In the sections below, we’ll dive deeper into why companies outsource to CROs, how CRO services function across each stage of drug development, who the key stakeholders are in a CRO-run project, emerging trends in 2025 for clinical trials outsourcing, the benefits and challenges of CRO partnerships, and tips on selecting the right CRO.
Why Outsource to CROs?
Pharmaceutical and biotech companies increasingly outsource clinical trials and research projects to CROs to leverage several strategic benefits. Key advantages of partnering with CRO companies include:
- Speed and Efficiency: A qualified CRO brings established processes, experienced staff, and ready infrastructure to hit the ground running. This can accelerate study start-up and execution timelines. Sponsors can focus on strategic decision-making while the CRO handles operational execution across all trial stages [8] [9]. By tapping into a CRO’s pre-existing systems for project management, data collection, and patient care, companies avoid “reinventing the wheel” for each trial and can complete studies more quickly and efficiently [10].
- Cost-Effectiveness: Outsourcing can convert fixed costs into variable costs, potentially lowering the overall R&D expense. Hiring a CRO often saves time and money – the sponsor avoids the expense of building in-house capabilities for every function of development [11]. Instead of maintaining large permanent teams that might be underutilized, companies pay for services only as needed. Studies show that by outsourcing to CROs, firms can reduce capital expenditures and shorten development timelines [12]. The CRO’s economies of scale (e.g. running many trials) can also drive cost efficiencies that are passed on to sponsors.
- Global Reach and Patient Access: Major CROs have a presence in numerous countries and deep knowledge of international clinical trial regulations [13]. This global footprint allows sponsors to conduct trials across North America, Europe, Asia, and emerging markets without having to establish offices in each region. CROs also maintain networks of investigational sites and relationships with the best trial investigators, which helps achieve high patient enrollment and access diverse patient populations [14] [15]. In an era where multi-regional trials are common and patient recruitment is a frequent bottleneck, a CRO’s global site network and recruitment specialists are invaluable for reaching enrollment targets faster.
- Specialized Expertise: CRO companies accumulate extensive experience across therapeutic areas and trial phases by running studies for many sponsors. They employ experts in fields like oncology, cardiology, rare diseases, etc., as well as functional experts in biostatistics, pharmacokinetics, data science, and regulatory affairs. Sponsors, especially small biotechs, leverage this external expertise to design more robust trials and navigate complex regulatory requirements. For instance, a CRO’s regulatory affairs team can help ensure a trial protocol meets FDA/EMA expectations, and its biostatisticians can optimize study design (e.g. sample size calculations or adaptive design methods). This depth of knowledge may exceed what the sponsor has internally, thus improving the quality and compliance of the trial.
- Flexibility and Focus: Outsourcing provides operational flexibility. Companies can scale research capacity up or down quickly by engaging CRO resources as projects demand, without the long lead time of hiring and training new internal staff. This agility is especially beneficial for small and mid-sized firms that have a few key trials – they can execute even large Phase III studies by partnering with a big CRO, then ramp down after completion. Meanwhile, the sponsor’s internal teams can focus on core competencies like drug discovery, pipeline strategy, or marketing, rather than being stretched thin managing every aspect of clinical development [16]. By delegating the heavy operational workload to a trusted CRO, the sponsor’s scientists and managers concentrate on the science and decision-making that only they can do.
In short, CRO services offer a potent combination of speed, cost-efficiency, global capabilities, and expert know-how that can significantly enhance a drug developer’s capacity to run trials. These benefits explain why the majority of pharmaceutical companies – from virtual biotechs up to Big Pharma – incorporate clinical trials outsourcing as a core part of their R&D strategy.
How CRO Services Support the Drug Development Lifecycle
CRO companies can contribute at virtually every stage of drug development, from early preclinical research through post-approval studies. Below is an overview of how CRO services typically operate across the drug-development lifecycle:
Preclinical Research Support (Drug Discovery to IND-Enabling Studies)
In the preclinical stage, CROs assist with laboratory and animal studies that evaluate a molecule’s safety and biological activity before human trials. Preclinical CRO services often include in-vitro assays (e.g. screening compounds for activity at the target, assessing ADME – absorption, distribution, metabolism, excretion profiles) and in-vivo studies (animal pharmacology and toxicology). Many CROs maintain GLP-compliant laboratories and animal research facilities to conduct these studies. For example, a sponsor might hire a preclinical CRO to run a 28-day rodent toxicology study and gather the safety data required for an Investigational New Drug (IND) application.
Key preclinical offerings from CROs usually cover: synthesis and formulation of the drug candidate for testing; pharmacokinetic studies (to understand drug metabolism and bioavailability); toxicology studies in at least two species (to identify any organ toxicity or safety margins); and specialized models (such as efficacy testing in disease models if needed). By outsourcing preclinical work, companies can tap CROs that have specific technical models and expertise – for instance, CROs with humanized mouse models for oncology, or zebrafish screening platforms for early toxicology. Outsourcing this stage can also be cost-effective, as indicated by industry analyses that outsourcing preclinical R&D reduces capital needs and shortens timelines [17]. Once the CRO completes these studies and the results support safety, the sponsor uses the data to file an IND and move into clinical trials.
Clinical Trial Phases I–IV: End-to-End Trial Management
Clinical development is where CRO support is most established. For Phase I–III trials (and Phase IV post-marketing studies), a full-service CRO can handle the end-to-end execution of the study on behalf of the trial sponsor. This includes a wide array of activities in compliance with GCP (Good Clinical Practice):
- Study design and protocol development: CRO medical and statistical experts can collaborate with the sponsor to design the trial, calculate sample size, and write the protocol and informed consent documents. They ensure the design is scientifically sound and regulatory-compliant. Many CROs also assist in IRB/ethics committee submissions for protocol approval.
- Site selection and initiation: CROs identify investigative sites (hospitals, clinics) with the right patient population and track record. They perform site qualification, negotiate contracts, and handle regulatory documents. Once sites are selected, the CRO conducts site initiation visits to train site staff on the protocol and study procedures [18].
- Patient recruitment and enrollment: Using their site networks and outreach strategies, CROs support enrollment of patients. They may create advertising materials (approved by IRBs) and utilize patient databases or referrals to meet enrollment targets. Their knowledge of investigators and sites in specific regions allows them to target high-enrolling centers to keep trials on schedule [19].
- Clinical operations and monitoring: Throughout the trial, the CRO’s clinical research associates (CRAs) monitor each site to ensure protocol adherence, verify data accuracy against source medical records, and confirm that patient safety reporting is handled correctly [20]. Monitoring can be on-site and remote. The CRO project manager oversees the trial timeline and coordinates all operational aspects, providing regular status updates to the sponsor.
- Data management and biostatistics: CRO data management teams set up the clinical database (often an electronic data capture system), develop case report forms, and continuously manage incoming data. They perform data cleaning, query resolution with sites, and ultimately lock the database. Biostatisticians at the CRO then analyze the trial data per the statistical analysis plan, generating tables, figures, and listings. Statistical analysis and programming is a core CRO competency [21] [22].
- Pharmacovigilance and safety monitoring: CRO medical monitors and drug safety personnel track adverse events reported during the trial. They may run a medical monitoring hotline for investigators to contact regarding patient safety questions. Serious adverse events are processed and reported by the CRO’s pharmacovigilance unit to regulators as required [23]. This ensures patient safety signals are handled promptly across all sites.
- Medical writing and regulatory submissions: A CRO’s medical writing team will draft the clinical study report at trial completion, as well as other documents like protocol amendments, Investigator’s Brochures, and even components of regulatory submissions (NDA/BLA) if contracted [24]. They ensure the documentation meets ICH and regulatory guidelines. The CRO can also coordinate directly with regulatory authorities on the sponsor’s behalf – for instance, scheduling meetings or responding to queries.
- Phase IV and post-approval studies: After a drug is approved, CROs often manage Phase IV trials or observational studies. These real-world evidence (RWE) projects collect data on the drug’s effectiveness and safety in routine clinical practice. CROs have epidemiologists and late-phase specialists who run post-marketing safety surveillance, patient registries, and outcomes studies. They apply real-world data sources (e.g. electronic health records, claims databases) and digital tools to gather post-approval insights. Regulators like FDA have programs to encourage RWE use in regulatory decision-making [25], and CROs help sponsors design studies to meet those expectations.
Not every sponsor outsources all of the above functions – some might only need a CRO for monitoring and data management, for example. However, many large trials today are run on a turn-key basis by CROs, where the CRO handles the majority of trial duties from start to finish [26], under oversight from the sponsor. Importantly, even when delegating extensively, the sponsor retains ultimate responsibility for trial quality and compliance (more on oversight in a later section). Some sponsors opt for a hybrid approach, keeping certain tasks in-house (like medical monitoring or final data analysis) and outsourcing the rest.
Regulatory Affairs and Medical Writing
Beyond running experiments and trials, CRO companies also provide crucial support in regulatory affairs – helping sponsors navigate the complex regulatory environment throughout development. CRO regulatory specialists assist in preparing and submitting regulatory filings such as IND applications, Clinical Trial Applications (CTAs in Europe), and ethics committee dossiers. They ensure that the trial protocols, patient consent forms, investigator qualifications, and safety monitoring plans meet FDA, EMA, and ICH requirements. For instance, a CRO might compile an IND submission for a sponsor, including all preclinical data, the trial protocol, investigator information, and manufacturing details, formatted according to FDA guidelines.
During a clinical trial, CRO regulatory teams manage communications with authorities (for example, reporting serious adverse events to FDA within required timelines, or submitting annual IND reports). They also coordinate inspections and audits – many CROs have internal quality assurance (QA) units that perform mock audits of trial sites and internal processes to ensure readiness for health authority inspections.
Medical writing is another core CRO offering. CRO medical writers prepare a range of documents: study protocols, investigator brochures, informed consent templates, monitoring plans, statistical analysis plans, clinical study reports, and journal manuscripts. A critical milestone is the clinical study report (CSR) which a CRO writes after trial completion, detailing methods and results; this becomes part of the regulatory submission for drug approval. CRO writers are adept at presenting data in the format regulators expect (e.g. ICH E3-compliant CSRs) and often work with sponsor teams to finalize submission modules (like the clinical summary sections of an NDA). They may also handle publishing services, ensuring that electronic submissions (eCTD format) are correctly compiled for regulatory review.
By leveraging CRO regulatory and writing services, sponsors gain access to personnel who are intimately familiar with current guidelines and agency expectations. This can reduce the risk of delays or rejections due to format or content issues in submissions. It’s especially valuable for smaller companies that might be filing their first drug application and want experienced professionals to guide them.
Post-Marketing and Real-World Evidence (RWE) Services
After a drug reaches the market, the partnership with a CRO can continue into the post-marketing phase. Phase IV studies (also called post-authorization safety studies or PASS) are frequently outsourced to CROs. These may be large simple trials or observational studies to gather additional data on long-term safety, comparative effectiveness, or usage in broader populations. CROs recruit real-world patients through physicians and collect outcomes to help sponsors and regulators understand how the drug performs outside the controlled trial setting.
In recent years, Real-World Evidence (RWE) has gained prominence. RWE refers to clinical evidence about a product’s use and benefits/risks derived from analysis of real-world data (RWD) – such as electronic health records, insurance claims, patient registries, or wearable device data [27]. CROs have developed dedicated RWE units to design and execute studies utilizing these data sources. For example, a CRO might run a retrospective database study to investigate incidence of adverse events, or a prospective registry to track patient-reported outcomes for a therapy over 5 years.
CRO capabilities in this realm include epidemiology study design, biostatistics for observational data, data linkage and analytics, and health economics outcomes research (HEOR). They also handle the compliance aspects (ensuring patient privacy, obtaining any needed consent or data-use agreements). The advantage for sponsors is that CROs can efficiently harness large real-world datasets and emerging digital health tools – such as smartphone apps or wearable biosensors – to capture data continuously from patients. Indeed, digital technology is enabling more remote data collection: for instance, CROs can deploy wearable devices and mobile apps to gather patient vital signs or symptoms in real time, feeding into RWE studies [28]. Regulatory agencies have begun accepting RWE to support label expansions or fulfill post-marketing commitments, making these CRO services increasingly strategic.
CRO Engagement Models: Full-Service vs. Functional Service Provider (FSP) vs. Hybrid
When outsourcing to CROs, sponsors can choose different business models for the partnership. The main models are:
- Full-Service Outsourcing (FSO): The sponsor contracts a CRO to handle all aspects of a clinical trial or development program, essentially end-to-end (full service). The CRO is responsible for the full study operations, and the sponsor’s involvement is primarily oversight and decision-making. Full-service CRO contracts are common for smaller companies lacking internal infrastructure, or when a sponsor wants one accountable party for the trial. The benefit is convenience and integrated management, but the challenge can be less direct control for the sponsor [29].
- Functional Service Provider (FSP): In an FSP model, the sponsor outsources specific functional tasks or departments to a CRO (or multiple CROs), rather than the whole trial. For example, a sponsor might use an FSP for all data management and biostatistics on its studies, or contract an FSP to provide all the clinical monitoring staff. This model allows the sponsor to mix and match expertise and retain more control over strategy and oversight of the trial, since the sponsor may still manage the overall project and protocol. FSP relationships are often longer-term (spanning multiple studies) and involve integrating the CRO’s personnel into the sponsor’s processes. In practice, many large pharma companies now use FSPs for ongoing support in data management, pharmacovigilance, etc., to flexibly extend their teams.
- Hybrid models: A hybrid approach combines elements of full-service and FSP. For instance, a sponsor might outsource entire trials on a full-service basis for some programs, while using an FSP approach for specific functions across the portfolio. Or the sponsor may use a hybrid FSP/FSO arrangement for a single trial – perhaps the CRO handles most trial conduct but the sponsor keeps certain pieces in-house or with a different vendor. Hybrid models aim to strike a balance between control and efficiency, tailoring the outsourcing to the sponsor’s strengths. In recent years, many sponsors have shifted to hybrid models to gain flexibility. Surveys indicate that nearly 90% of drug developers utilize either FSP or hybrid outsourcing models for most of their clinical development needs, and FSP-style partnerships are growing faster than traditional full-service deals [30] [31]. In one industry survey, 41% of respondents had increased use of FSP outsourcing (versus 27% for full-service outsourcing), reflecting this trend toward more customized partnership models [32].
Each model has pros and cons. Full-service offers simplicity (one CRO accountable for results) but can reduce sponsor’s direct oversight on daily operations [33]. FSP provides flexibility and sponsor oversight but requires more coordination on the sponsor’s side (managing multiple functional vendors). The optimal choice depends on the sponsor’s internal capabilities, preference for control, and the complexity of the project. It’s not uncommon for big sponsors to maintain strategic partnerships with a few global CROs that can do full-service, while simultaneously having FSP contracts for particular specialties.
Regardless of model, clarity in roles and communication is key. Sponsors often establish governance structures with CRO partners – for example, joint operating committees and clear escalation paths – to manage the relationship whether it’s full-service or FSP. The next section describes how the various stakeholders collaborate in a typical sponsor-CRO project workflow.
Stakeholders and Workflow in a Sponsor–CRO Collaboration
When a company outsources a clinical trial to a CRO, several stakeholders work in concert to execute the project. At a high level, the key parties include the sponsor (the company developing the drug), the CRO project team (led by a project manager, with functional leads for clinical operations, data, etc.), trial site staff (investigators and study coordinators at hospitals/clinics), and oversight functions like quality assurance. Below is a high-level timeline of how a clinical trial progresses with a CRO, highlighting roles at each stage:
- Planning and Vendor Selection: The process begins with the sponsor defining the trial’s scope and objectives. The sponsor then selects a CRO through a request for proposal (RFP) and bid defense process. Once a CRO is chosen, both parties hold a kickoff meeting to align on the plan. The sponsor’s team (e.g. clinical program manager and medical lead) works with the CRO Project Manager (PM) to review the protocol, milestones, and responsibilities. A detailed work plan and quality agreement are established, outlining who does what and performance expectations. At this stage, the sponsor will formally delegate trial duties to the CRO in writing (per regulations like FDA 21 CFR 312.52), but the sponsor also sets up an oversight plan to monitor CRO performance.
- Study Startup: The CRO’s clinical operations group takes the lead in study startup activities. This includes site identification and activation: the CRO, with sponsor input, identifies investigative sites and manages site contracts and ethics approvals. The CRO’s regulatory specialists prepare submissions to IRBs/ethics committees and any required regulatory authority approvals (such as a Clinical Trial Application in Europe). Meanwhile, the CRO’s data management team builds the study database and electronic data capture (EDC) forms. Throughout startup, the CRO PM coordinates tasks and timelines, while the sponsor’s project representative tracks progress in oversight meetings. Quality Assurance (QA) personnel may review critical documents (like the monitoring plan or data management plan) to ensure they meet GCP and the sponsor’s standards before site initiation.
- Trial Conduct (Enrollment to Monitoring): Once sites are initiated, the trial moves into execution. Investigators and site staff begin recruiting and treating patients per the protocol. The CRO deploys its Clinical Research Associates (CRAs) to monitor each site—checking informed consent documentation, verifying data entries against source records, and ensuring protocol compliance. The CRO Data Management team receives case report form data and runs edit checks, querying sites for clarifications as needed. The sponsor and CRO typically have weekly or biweekly project team meetings during this phase to review enrollment status, data quality, and any issues. The CRO PM is the point person for daily operations, issue resolution, and status reporting to the sponsor. The sponsor’s role here is primarily oversight: reviewing progress reports, monitoring quality metrics, and providing medical or scientific guidance when protocol questions arise. The sponsor’s pharmacovigilance unit (or the CRO’s, if delegated) reviews incoming adverse event reports for any safety signals. If interim analyses or Data Monitoring Committees are planned, the CRO biostatistics team prepares the data cuts and analyses, which the sponsor and committee review. QA audits may be conducted during the trial (e.g. the sponsor’s QA might audit a high-enrolling site or audit the CRO’s trial master file) to ensure compliance. Throughout, the sponsor remains responsible for making decisions on protocol modifications or resource adjustments, while the CRO executes the agreed plan.
- Data Analysis and Reporting: After the last patient completes treatment and follow-up, the study winds down. The CRO performs a thorough database clean-up and lock. All queries are resolved, and no further changes to data are allowed after lock. The CRO’s biostatisticians then generate the final analysis per the statistical analysis plan. Tables and figures of efficacy and safety results are produced. The CRO’s medical writing team, in collaboration with sponsor medical experts, drafts the Clinical Study Report (CSR) summarizing the trial methods and outcomes. During this stage, the sponsor remains engaged by reviewing and approving the analysis outputs and report drafts. The sponsor’s input is critical to ensure the report accurately reflects the data and supports the sponsor’s regulatory strategy. The CRO PM coordinates the assembly of all necessary documentation (data listings, appendices, audit certificates, etc.). If the trial is pivotal for a marketing application, the CRO may also assist in preparing submission-ready datasets and integration into the Common Technical Document (CTD) format. This phase ends with delivery of the final CSR and dataset to the sponsor. A formal closeout meeting is often held to review performance, milestones met, and any lessons learned.
- Study Close-Out and Follow-Up: The last step involves wrapping up trial operations. The CRO helps close out each site – CRAs conduct site close-out visits to ensure all documentation is complete, investigational product is accounted for or destroyed, and any outstanding queries are resolved. The CRO ensures the trial master file (TMF) is complete and archived (often now an electronic TMF). The sponsor may request a QA audit of the final TMF to verify its completeness. If the sponsor is filing for drug approval, the CRO might continue providing support by addressing any regulatory questions that arise about the trial data. Additionally, the CRO can transition into post-marketing activities (if contracted), such as facilitating publication of results or starting a Phase IV study or registry.
Throughout this timeline, communication and oversight are the linchpins of a successful sponsor-CRO collaboration. The sponsor typically assigns a project liaison or oversight manager who keeps in close contact with the CRO PM. Both sides track key performance indicators: enrollment rates, data query turnaround time, protocol deviation counts, etc. If issues arise (e.g. slow enrollment at a site, data entry backlogs), the CRO proposes and implements mitigations, but the sponsor is kept informed and approves any major changes. Regulatory compliance is jointly monitored – for example, ensuring GCP guidelines are followed and that the CRO complies with all delegated responsibilities. Notably, ICH GCP (E6 R2) explicitly states that even when responsibilities are transferred to a CRO, “the sponsor should ensure oversight of any trial-related duties and functions carried out on its behalf” [34]. Thus, the sponsor must actively oversee the CRO’s work (through reports, audits, co-monitoring visits, etc.) and remain accountable for the trial’s integrity.
By adhering to a clear workflow and delineation of roles as above, sponsors and CROs can successfully execute trials with high efficiency and quality. The CRO handles the heavy operational lift, and the sponsor provides governance and scientific leadership. Next, we’ll look at current trends shaping how CROs operate in 2025 and beyond.
2025 Trends in Clinical Trials Outsourcing and CRO Innovation
The clinical research landscape is evolving rapidly, and CRO services are at the forefront of innovation. In 2025, several key trends and new practices are influencing how CRO companies work and how trials are conducted:
- Decentralized and Hybrid Trials: The COVID-19 pandemic accelerated adoption of decentralized clinical trial (DCT) approaches, and these remain a strong trend in 2025. Decentralized trials use digital technology and local healthcare providers to reduce the need for patients to travel to central sites. For example, visits may be conducted via telemedicine or home nursing, and mobile health devices can transmit patient data remotely. CROs are heavily investing in DCT capabilities – building networks of traveling nurses, partnering with telehealth providers, and deploying remote monitoring platforms. Regulators support this trend: FDA guidance in 2023 outlined how decentralized trial elements can improve patient access and diversity in trials [35] [36]. By 2025, it’s common for CROs to offer “hybrid” trial solutions that combine traditional sites with remote components. This results in more patient-centric studies and often faster enrollment, since geography is less of a barrier. According to industry outlooks, decentralized trial elements will continue to expand, making trials more flexible and inclusive for patients [37].
- AI-Driven Recruitment and Data Analytics: Artificial intelligence (AI) and machine learning tools are being applied by CROs to streamline various aspects of trials. One high-impact area is patient recruitment – AI algorithms can mine electronic health records or social media to identify potential trial candidates more efficiently than traditional advertising. AI can match patient eligibility criteria with databases of millions of patient records to find those likely to qualify, dramatically shortening recruitment timelines. There are also AI-driven approaches to creating synthetic control arms (using historical patient data to serve as a control group), which some CROs are piloting to reduce the need for enrolling placebo patients [38]. Additionally, AI is used in drug trial design (simulating outcomes under different protocols to select an optimal design) and in data cleaning (identifying anomalies in datasets). In 2024, the number of trials utilizing AI tools hit record levels [39]. By 2025, sponsors expect CROs to bring data science innovations to the table. For example, a CRO might use machine learning to predict which sites will enroll best or to flag risk of patient drop-out so that interventions can be taken. These technologies all aim to make trials faster, more reliable, and cost-effective. Early evidence suggests AI can indeed increase recruitment efficiency and cut trial costs when implemented well [40].
- Adaptive Trial Designs: Hand-in-hand with AI, there’s a push toward more adaptive trial designs in clinical development. Adaptive trials allow pre-planned modifications to the trial (such as dose adjustments, sample size re-estimation, or dropping/adding treatment arms) based on interim data analyses, rather than sticking to a fixed design. CRO biostatistics teams are well-versed in planning and executing adaptive trials, which require complex simulation upfront and careful governance to maintain validity. In 2025, adaptive designs are especially prevalent in oncology and rare disease trials, where they can streamline development by accelerating decision-making on ineffective treatments [41]. For instance, a seamless Phase II/III adaptive trial might let a sponsor transition to Phase III and expand patient numbers as soon as early results look promising, instead of stopping and starting a new trial. Regulatory agencies have put out guidance encouraging adaptive approaches in certain contexts, and CROs have responded by developing statistical toolkits for these designs. The result is often reduced trial durations and resource use, as adaptations help focus on the best-performing treatment arms.
- Emphasis on ESG and Sustainability: The focus on Environmental, Social, and Governance (ESG) compliance has grown within clinical research operations. Sponsors are now interested in the sustainability practices of their CRO partners. This includes how CROs manage trial waste, whether they have green initiatives (for example, reducing business travel emissions by using remote monitoring technologies), and how they ensure ethical conduct and diversity. In fact, diversity in trial populations is both a scientific and ESG concern – ensuring trials are equitable and inclusive. Regulators and industry groups have set expectations for trial diversity, and decentralized methods (noted above) are one way CROs help achieve that. On the environmental side, leading CROs have started reporting their carbon footprints and making commitments to reduce them. For example, some CROs cut tens of thousands of air-travel miles by utilizing regional monitoring and video visits, significantly reducing CO₂ emissions [42]. By 2025, many sponsors include ESG criteria in CRO selection, favoring partners who demonstrate sustainable practices and strong governance. The industry outlook is that sustainability and diversity will remain critical priorities, driven by regulatory mandates and company commitments [43]. In practice, this means CROs are implementing greener workflows (digital documents instead of paper, smarter logistics for lab samples, etc.) and fostering patient diversity initiatives (community outreach programs, multilingual patient materials, etc.) as part of their service value.
- Wearables and Digital Health Integration: The rise of wearable devices and remote monitoring technology is transforming data collection in trials. Modern CROs routinely incorporate digital health tools – such as continuous glucose monitors, smartwatches, blood pressure cuffs, or activity trackers – into study protocols to gather real-world patient data in between clinic visits. These devices feed rich datasets on patient physiology and behavior, enhancing the evaluation of a drug’s effects. For example, a wearable ECG patch might continuously monitor a cardiac patient’s heart rhythm during a trial, potentially detecting safety signals that periodic clinic ECGs might miss. CROs have developed platforms to manage the influx of data from such devices and ensure it’s securely transmitted and integrated into the study database. The FDA’s guidance on digital health technologies in DCTs (2023) highlighted that wearable sensors can allow more frequent or continuous data collection, yielding more robust data sets for analysis [44]. By 2025, it’s become almost standard for Phase I and II trials to use some form of digital biomarker or remote patient monitoring. CROs differentiate themselves by the quality of their technology ecosystem – offering sponsors user-friendly apps for patient-reported outcomes, BYOD (bring-your-own-device) solutions for data capture, and analytics to make sense of the high-volume data streams from wearables. This tech-driven approach not only improves data quantity, but also enhances patient engagement (patients can participate from home with reminders and feedback via apps).
Overall, these trends indicate that CRO companies are continuously innovating to improve trial speed, data quality, patient centricity, and compliance. A term sometimes used is “CRO 2.0,” reflecting a more digital and patient-focused contract research model. Sponsors evaluating CRO partners in 2025 are thus considering not just operational capacity, but also whether a CRO is up-to-date with these innovations – can they run a hybrid decentralized trial? Do they utilize AI for efficiency? Are they aligned with our values on sustainability? The CRO landscape is competitive, and those that adapt to these trends stand out as preferred partners.
Benefits and Challenges of CRO Partnerships
Outsourcing drug development to a CRO offers many benefits, as discussed earlier, but it also comes with challenges that sponsors must actively manage. It’s important to weigh the operational flexibility against potential downsides like loss of direct control. Here we outline some key benefits and challenges of CRO partnerships:
Operational Flexibility and Scale: On the plus side, engaging CROs gives sponsors tremendous flexibility. You can rapidly scale up a development program by leveraging a CRO’s workforce – for example, starting a large global Phase III trial in months by using an established CRO infrastructure, which would take years for a small biotech to build on its own. If priorities change, you can also scale down just as easily by ending a contract, without dealing with layoffs or unused facilities. This flexibility enables a sponsor to pursue more projects in parallel and adapt to pipeline changes. CRO partnerships also allow a broader geographic reach instantly, as CROs have offices and staff worldwide. This is a powerful benefit for running global trials or tapping patient populations in specific regions (CROs know how to operate in, say, Latin America or Southeast Asia, far better than a new sponsor would). Moreover, a strategic CRO alliance can become a long-term extension of the company – some pharma companies have preferred-provider agreements where a CRO essentially becomes an external department for them, deeply familiar with their products and standards.
Expertise and Speed vs. Oversight and Quality Control: A major challenge in CRO partnerships is ensuring that the outsourced activities meet the sponsor’s quality standards and regulatory obligations. When you outsource, you inherently relinquish some direct control over day-to-day activities. The CRO’s team will be making many decisions in the field. If not properly managed, this can lead to issues – for instance, inconsistent trial enrollment efforts or variable data quality across sites. Maintaining oversight is critical. Regulatory guidelines make it clear that sponsors cannot outsource responsibility: even if a CRO is doing the work, the sponsor is accountable for trial conduct and data integrity [45]. This means sponsors must invest time in oversight activities like co-monitoring visits, data reviews, and regular governance meetings. Failure to oversee can result in unpleasant surprises – there are cases where sponsors discovered protocol deviations or data problems late because they relied blindly on a CRO. In fact, surveys have found that only about one-third of sponsors feel they have fully achieved their goals with CRO engagements, indicating room for improvement in managing these partnerships [46]. The takeaway is that while CROs bring expertise and speed, sponsors must actively manage the collaboration to maintain quality. Clear communication, defined KPIs, and a robust oversight plan mitigate this challenge.
Intellectual Property (IP) and Confidentiality: Another concern is protecting sensitive information. When working with a CRO, sponsors inevitably have to share proprietary data, such as molecular structures, unpublished results, or strategic plans. Reputable CROs have strict confidentiality agreements and data security measures in place, but the sponsor should conduct due diligence on these aspects. There is a small risk of IP leakage or conflicts of interest (e.g. the same CRO working with a competitor). Sponsors can address this by including confidentiality and intellectual property clauses in contracts (ensuring data and inventions arising from the collaboration belong to the sponsor) and by choosing CROs with a strong ethical track record. It’s also wise to verify that the CRO’s IT systems and processes comply with data protection standards. In today’s environment of cybersecurity risks, a lapse on the CRO side could expose trial data. Thus, part of the challenge is to trust but verify – trust the CRO as a partner, but verify that IP safeguards and data security are robust.
Communication and Cultural Alignment: Collaborating closely with an external organization can introduce communication challenges. The CRO’s team and the sponsor’s team need to function as one unit despite different company cultures and possibly time zones. Miscommunications or misaligned expectations can lead to errors or delays. For example, if the sponsor assumes the CRO is handling something that the contract didn’t explicitly cover (or vice versa), tasks can fall through the cracks. To prevent this, successful partnerships emphasize transparency and frequent communication. Many sponsors involve CRO staff in their internal project meetings and use collaborative project-management tools to share information in real time. It’s also beneficial when there is a good cultural fit between sponsor and CRO – similar philosophies on quality, agility, and problem-solving. Some large CROs might feel bureaucratic to a nimble biotech, for instance, leading to frustration. Therefore, selecting a CRO that matches the sponsor’s working style can mitigate this challenge. With effort on both sides, a CRO can essentially function as an extension of the sponsor’s team.
In summary, CRO partnerships bring great benefits – expanded capabilities, faster timelines, cost savings – but they require diligent management of challenges like oversight, quality control, and communication. The sponsor must remain actively engaged. Many sponsors develop internal competencies in vendor management to maximize the value from CROs. When done right, the contract research organization becomes a true strategic ally in bringing a new therapy to market. But if handled poorly, outsourcing can result in costly delays or quality issues. By understanding these trade-offs and planning accordingly, companies can enjoy the upside of CRO collaborations while controlling the risks.
How to Choose the Right CRO: Key Selection Criteria for Sponsors
Choosing the right pharmaceutical CRO partner is a critical decision that can influence the success of a drug development project. Not all CRO companies are equal in capability or quality, so sponsors should evaluate candidates against clear criteria. Here are important selection factors and due-diligence steps when considering a CRO:
- Compliance and Quality Track Record: Verify the CRO’s GCP compliance history and quality standards. Sponsors should inquire about the CRO’s past FDA or EMA inspections – have they been inspected for trials, and if so, were there any major findings or warning letters? A strong CRO will have a clean compliance record or have effectively remedied any past issues. Ask about their internal quality assurance processes (Do they do internal audits? How do they qualify their own vendors and sites?). You can request summaries of any regulatory audits or certifications. Essentially, you want assurance that the CRO follows ICH GCP guidelines rigorously and will uphold the same level of ethics and data integrity that your own team would.
- Therapeutic Area Expertise and Experience: Look for a CRO that has direct experience in the therapeutic area or study type of your project. For example, if you’re running an oncology trial, a CRO with a robust oncology division and relationships with cancer centers is advantageous. Examine the CRO’s track record: Have they done similar Phase II oncology trials? What were the outcomes (e.g., met enrollment timelines, data accepted by FDA)? The CRO should be able to provide case studies or client references in your indication. Also consider any specialized needs of your trial – such as advanced therapy expertise (gene therapy trials), pediatric trial experience, or ability to run preclinical GLP studies if that’s in scope. A CRO that deeply understands the disease area can anticipate challenges and apply proven solutions, acting truly as a scientific partner.
- Scope of Services and Technology Capabilities: Depending on your needs, decide if you want a full-service CRO or if you will source different services separately. If you prefer one partner for efficiency, ensure the CRO offers all the services you require at high quality – from protocol development and patient recruitment to lab services and data management. Evaluate their technology: Do they use modern electronic data capture and eTMF (electronic trial master file) systems? Are their data management and analysis tools robust and validated? If decentralized trial elements or complex biomarkers are part of your trial, can the CRO support those (for instance, do they have remote monitoring platforms, or lab partnerships for specialized assays)? Sponsors should ask for a demonstration of the CRO’s clinical trial management system or data platforms to see if they meet expectations. A tech-savvy CRO can bring efficiencies and better data visualization to your study.
- Geographic Footprint and Site Networks: The geographic reach of the CRO should match the trial’s requirements. If your trial needs global enrollment, choose a CRO with operations (offices or affiliates) in those target countries and knowledge of local regulatory processes. They should have multilingual staff and familiarity with regional patient recruitment channels. Global trials also benefit from CROs that have established site networks or preferred site relationships in each region – this can accelerate site start-up. On the other hand, if your trial is only in one country or region, a smaller regional CRO might suffice (and could be more cost-effective). The key is to ensure the CRO has access to the patient population you need. During selection, ask how many trials they’ve done in the countries of interest and how quickly they typically enroll there. A CRO’s past performance metrics by region can be very telling.
- Project Team and Communication: The qualifications of the project team the CRO assigns are crucial. Meet (virtually or in person) the proposed Project Manager and key functional leads (lead CRA, lead data manager, etc.) during the bidding process. Their expertise, communication style, and commitment can make or break the trial. Sponsors should assess: Does the PM have sufficient experience with similar studies? Are they managing a reasonable number of other projects (not over-allocated)? Also gauge the CRO’s communication practices – will there be regular update calls, what reports will they provide, is there a single point of contact or multiple? Effective communication and a good rapport with the CRO team will help navigate issues during the trial. It’s often said that you’re not just choosing a company, you’re choosing the specific people who will run your study. Ensure you’re comfortable with the team’s competence and dynamics.
- Cost and Transparency: While not the only factor, cost is important. Scrutinize the CRO’s budget proposal for transparency and completeness. A reputable CRO should provide a detailed cost breakdown by activity (project management, monitoring, lab tests, etc.) and assumptions (number of sites, patients, monitoring visits). Be cautious of budgets that are significantly lower than competitors – they may be underestimating tasks or planning to change-order you later. Conversely, the highest bid isn’t always the best quality, so weigh cost against the above factors. Look for cost transparency: ask how the CRO handles changes in scope (e.g. if enrollment extends, how will budget be adjusted?). It’s also wise to clarify payment terms and milestones. Some sponsors opt for unit-based contracts (pay per patient enrolled or per visit) to ensure payment aligns with performance. Ultimately, choose a CRO that is financially stable and offers fair pricing with no hidden fees. A good partnership will involve some flexibility on both sides to accommodate unforeseen changes without excessive penalties.
- Client References and Reputation: Do due diligence on the CRO’s reputation. Request references from other sponsor clients and actually call them to ask about their experience. You can also check industry reports or rankings (e.g., CenterWatch or ISR reports that survey sponsors’ CRO satisfaction). Consistently positive feedback on delivery, personnel, and flexibility is a green flag. If you encounter red flags – like reports of poor communication or missed deadlines – discuss these with the CRO for their explanation. Additionally, ensure the CRO isn’t overextended with too many projects; a company taking on more than it can handle may not give your trial sufficient attention. Sometimes mid-sized CROs can offer more personalized service compared to the largest CROs, which might assign smaller clients lower priority. So, fit-for-purpose size and attention is a consideration. In recent surveys, many biotechs favor mid-sized CROs for their nimbleness and focus [47].
In summary, selecting a CRO requires balancing hard data (experience, capabilities, metrics) with soft factors (culture fit, communication). It’s wise to involve cross-functional team members in the vetting process – medical, regulatory, data, etc. – to evaluate the CRO from all angles. Treat it almost like a job interview for a key position in your organization. After all, the CRO will be handling your valuable trial and patients. Taking the time to choose the right partner will pay off in smoother execution.
Lastly, remember that there are resources to aid your search. Online platforms are emerging to connect sponsors with vetted service providers. Pharmaoffer now hosts a growing roster of vetted CRO providers that visitors can filter and contact based on molecule, region, or service specialty. Such tools can help you shortlist candidates that fit your project’s needs, especially if you’re new to pharma outsourcing. By applying rigorous selection criteria and leveraging available information, you can find a CRO partner that aligns with your goals and values.
Conclusion
In today’s pharmaceutical R&D environment, CRO companies have become indispensable drug-development partners. They offer the operational muscle, specialized expertise, and global reach needed to bring new therapies from bench to bedside efficiently. Understanding how CRO services work – from preclinical experiments to clinical trials and regulatory support – allows sponsors to collaborate more effectively and tap into these benefits. While outsourcing introduces new oversight responsibilities for sponsors, the rewards of faster development and cost savings are well worth it when managed properly. By choosing the right Contract Research Organization and maintaining a strong partnership, pharmaceutical innovators can accelerate their clinical programs and ultimately deliver new treatments to patients sooner. CROs are, in many ways, catalysts in the drug development journey – when you find the right one, they truly work as an extension of your team, turning scientific plans into tangible results. With clear expectations, communication, and shared commitment to quality, a sponsor-CRO collaboration can be a powerful engine driving success in clinical development
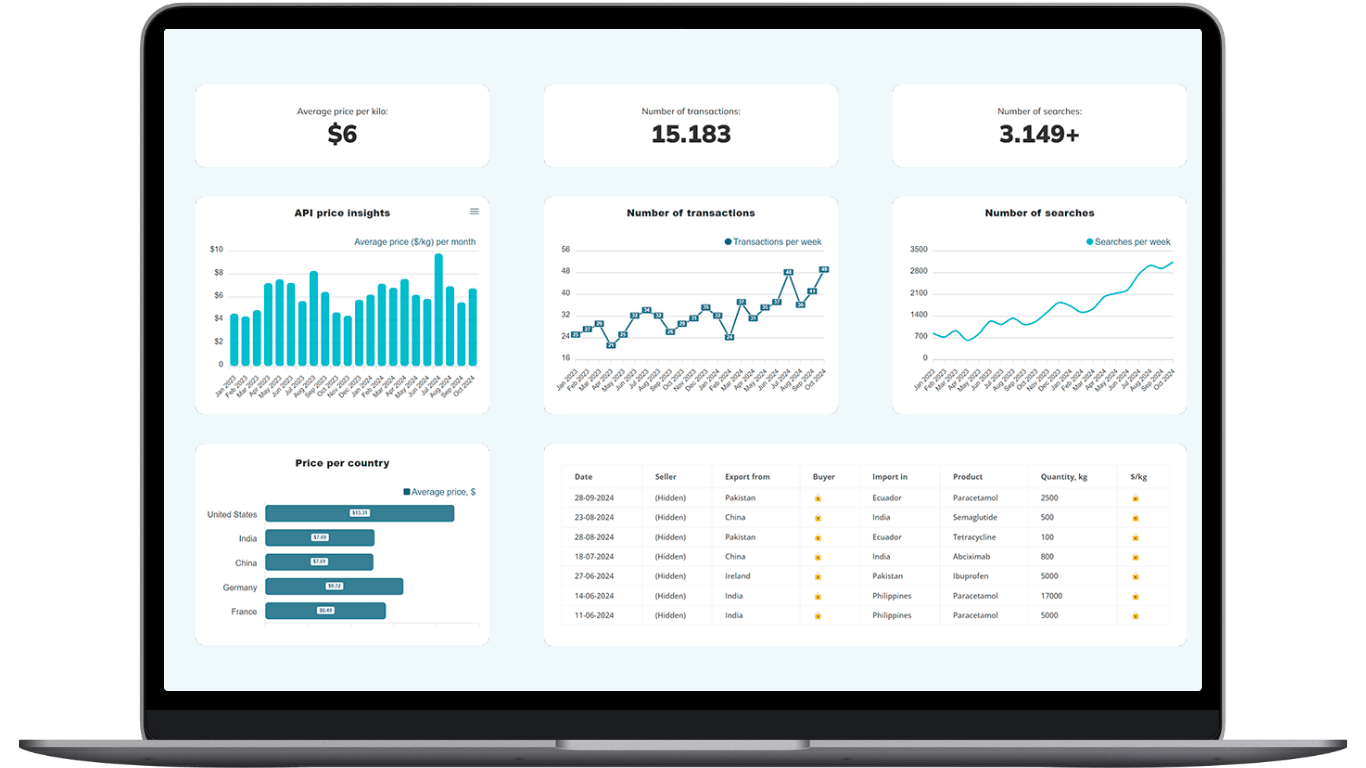
Make Smarter API Decisions with Data
Access exclusive insights on global API pricing, export/import transactions, competitor activities and market intelligence.
What is a Contract Research Organization (CRO) in the pharmaceutical industry?
A Contract Research Organization is an independent company that pharmaceutical, biotech or medical-device sponsors hire to plan, run and analyze studies across the drug-development lifecycle, from preclinical safety tests through Phase I-IV clinical trials and post-marketing surveillance. CRO services typically include study protocol design, site selection, patient recruitment, clinical monitoring, data management, biostatistics, regulatory-affairs support and medical writing. Using a pharmaceutical CRO lets sponsors tap proven infrastructure and expertise without building it all in-house, which is why CRO companies have become a US $50 billion global sector.
Why do pharma and biotech companies outsource clinical trials to CRO companies?
Sponsors outsource for four main reasons: speed (CROs can launch studies faster with ready staff and sites); cost control (outsourcing converts fixed head-count into variable fees and leverages CRO economies of scale); global patient reach through the CRO’s international site networks; and access to specialised therapeutic and regulatory expertise that smaller firms may lack internally.
Which services does a full-service CRO provide during drug development?
A full-service pharmaceutical CRO can cover every phase:
- Preclinical studies (ADME, in-vitro & in-vivo tox)
- Clinical Phases I-III—site contracting, monitoring, data capture and safety reporting
- Phase IV & real-world evidence programmes after approval
- Regulatory-affairs support (IND/CTA prep, agency meetings) plus medical writing for protocols and clinical study reports
Because everything sits under one roof, sponsors can streamline timelines and maintain a single set of KPIs across the programme, making full-service CROs a popular model for clinical trials outsourcing
How can sponsors choose the right CRO partner for their study?
Evaluate five pillars: (1) GCP compliance record and recent FDA/EMA inspection outcomes; (2) proven therapeutic-area expertise and past performance metrics in similar trials; (3) geographic footprint and site networks that match your enrolment plan; (4) technology stack—EDC, eTMF, decentralised-trial capabilities and data security standards; and (5) transparent budgeting plus communication style that aligns with your team’s culture. Platforms like Pharmaoffer let you filter vetted CRO services by molecule, region and certification to create a targeted shortlist quickly.
What CRO service trends should sponsors watch in 2025?
Five hot trends are shaping CRO services:
- Decentralised and hybrid trials that bring visits to the patient via telehealth and home nurses, backed by new FDA guidance in 2023.
- AI-driven patient recruitment and data analytics, which leading CROs use to find eligible participants faster and mine sub-populations in big datasets.
- Functional Service Provider (FSP) outsourcing models gaining share as sponsors mix in-house control with CRO scalability.
- Wearable and digital-health data capture to collect continuous real-world metrics and boost patient engagement.
- Growing focus on ESG, diversity and sustainability in trial operations as sponsors add these metrics to CRO selection scorecards.





Check out all other blogs here!