
Su Keles| Posted on December 27, 2022
Will 3D-printed medicine be a game changer in the pharma world?
What is personalized medicine?
Even though we all have different physical and genetic traits, most medicines we consume assume we are entirely the same. It’s a conventional medicine manufacturing system and can be described as: “one size fits all,” where most patients receive the same drugs at the same doses and frequencies as others. But as one can imagine, the restricting concept of “one size fits all” does not deliver efficient results for all treatments.
Administrating the same API at the same dose to different patients can lead to undesired responses. The response could be too strong or weak, resulting in either adverse drug reactions or no reactions. Thus, even though generics are essential and help millions of people, there is an easily seen shift toward personalization and customization of medicine.
Personalized medicine can be seen as the opposite of the “one size fits all” perspective. It can potentially revolutionize the healthcare industry by customizing medication to a specific individual. This will allow the drug to treat and focus only on that individual’s physiology and genetic characteristics and not the mass population. This leads to more precise and efficient medications, improving patient compliance. Personalized medicine sounds like a great alternative, but how do you create these tailored drugs? What are the benefits? How does it exactly work?
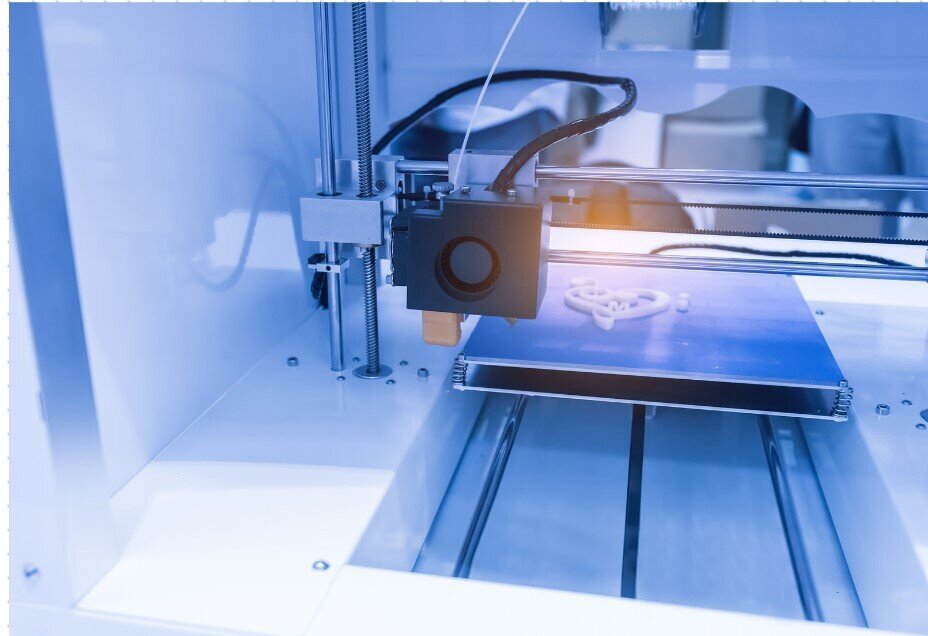
What is 3D printing?
Three decades ago, 3D printers were large and expensive. Over the last decade, costs have decreased so drastically that most hobbyists can afford their 3D printing machines.
It started with being widely used in the construction of buildings, but except for construction purposes, it is also being used in industries such as entertainment, fashion, and art. The pharmaceutical industry is now catching on with the trend; 3D printers have been used to produce various pharmaceutical products.
3D printing is the tool that makes personalized medicine a reality, thus improving patient compliance by tailoring the medication to the patient. The emergence of 3D printing allowed the idea of printable and personalized medicine to grow and develop into new opportunities to treat patients.
In 2015, the FDA (Food and Drug Administration) approved the first 3D-printed tablet. Spritam is a reformulation of the anti-epileptic seizure drug Levetiracetam. It has a specific structure that is not possible to achieve using traditional manufacturing methods. The success of Spritam attracted other pharmaceutical companies to invest time and money in developing 3D medicines, taking advantage of the main benefits such as shorter lead times, drug combinations, and lower costs.

Make Smarter API Decisions with Data
Access exclusive insights on global API pricing, export/import transactions, competitor activities and market intelligence.
Benefits of 3D-printed tailored medicine
The most significant benefits are the reduction of API (thanks to smaller badges, up to 50% can be saved on APIs) and the reduction of working hours (due to the flexibility of 3D printing in formulation, trading can be done up to 60% faster).
Furthermore, 3D printing has the advantage of producing on-demand and immediate medicines. It is especially beneficial and cost-effective for products with a limited shelf life. Also, parts of the world that do not have fair access to treatment could benefit from 3D printing, such as military operations, disaster areas, and even outside the world, like space missions.
The equipment cost is significantly lower than other automated production technologies. Free 3D modeling software is available online to anyone, making 3D printing of medications accessible with the simple purchase or lease of a 3D printer.
One of the other main benefits of 3D-printed medicine is the possibility of combining multiple drugs in one pill. Many people use various pills for different conditions, possibly at different times throughout the day. But taking the right pill at the right time is not as easy as it sounds, and it makes dangerous mistakes possible. It would be more convenient and safer if people could take just one pill that provides all the proper medication at the right time in the correct dose, called “polypills.” These polypills can contain many layers released at different times in the human body.
While producing these polypills in the “one size fits all” structure is costly and time-consuming, 3D printing technologies offer a cheaper alternative.
Potential risks of 3D-printed medicine
But 3D printed medicine doesn’t only come with benefits. Here are some examples of potential risks this new technology might face:
Firstly, traditional manufacturing facilities deal with intensive regulatory checks, which leaves little room for mistakes. However, the FDA can only partially regulate 3D printing, so controlling the safety of the products is more tricky. This leads pharmaceutical companies to mainly produce medicine with traditional methods since they can better monitor the drug development process from beginning to end.
But there is another big concern. Cyber risks can lead to an increase in counterfeit medicine. Printers are much more vulnerable to hackers than traditional manufacturing processes. For instance, hackers can alter a drug’s recipe within a hospital or pharmacy where it’s printed, leading to severe health consequences for patients. Or, in a relatively less serious situation, it can lead to the exploitation of intellectual property; a hacker can gain access to a medicine maker’s blueprint and bring it to a manufacturing plant overseas to mass produce the drug.
If you are curious about counterfeit medicines, check out this blog, where we dive deep into the world of falsified medicine.
But how does it exactly work?
3D printers add material, layer-by-layer, to form a 3D object. In a more precise way, 3D printing involves the development of a three-dimensional object in a layer-upon-layer manner using various computer software.
To keep it as simple as possible: the three most popular forms of 3D printing are fused deposition modeling (FDM), stereolithography (SLA), and selective laser sintering (SLS). SLS is mainly an industrial process, while FDM and SLA cover a higher range, from high-end manufacturing to simple desktop units.
An ideal 3D printer in a pharmacy setting should be easy to use. It should require minimal setup and training, save time compared to traditional compounding, and efficiently use approved pharmaceutical ingredients. Some printers seem close to reaching most of these goals, while others can better address only one.
Conclusion
This technology has been proven effective, yet 3D-printed medicine still has a long way ahead to reach its full potential and be commonly used worldwide. The FDA has approved only a few products since the initial one in 2015. More research and development are needed to fully discover the disruptive effects it can have on the pharmaceutical industry.
Thank you for reading!





Check out all other blogs here!