Vibegron API Manufacturers & Suppliers
Find, compare & contact
Filters
Custom request?
Type
Production region
Qualifications
Country of origin
Producer
Produced in:
Established in: 2019
MOQ: 1 kg
Employees: 10+

Focused on pharmaceutical industry

Reasonable price for the customers

Full service from R&D stage to commercial stage
+ 0
All certificates
Distributor
Produced in:
Established in: 2011
MOQ: -
Employees: 25

Technical expertise ensuring optimal selection and development of APIs and intermediates

Globally connected with multiple GMP-compliant manufacturing facilities

Regulatory excellence with a dedicated team with global reach
+ 0
All certificates
How does it work?
You can register for free as long as you are registering on behalf of a legal company related to the pharmaceutical industry
Search in the search bar the product that you’re looking for. We’ll show you an overview of all available suppliers. Use the filters to select the relevant suppliers only
Have you found interesting suppliers? Then it’s time to contact them. Use the send inquiry button and send them a message. You can send for each product, 3 inquiries per week
Suppliers get notified by Pharmaoffer that they’ve received a new inquiry. They will come back to you with their questions, certificates, and offer in the chat on Pharmaoffer. We will send you an email in case of any news
Does the supplier meet your quality and commercial requirements? Then you can place the order. Just follow the steps of our order module
Looking for Vibegron API 1190389-15-1?
- Description:
- Here you will find a list of producers, manufacturers and distributors of Vibegron. You can filter on certificates such as GMP, FDA, CEP, Written Confirmation and more. Send inquiries for free and get in direct contact with the supplier of your choice.
- API | Excipient name:
- Vibegron
- Synonyms:
- Vibégron , Vibegrón , Vibegronum
- Cas Number:
- 1190389-15-1
- DrugBank number:
- DB14895
- Unique Ingredient Identifier:
- M5TSE03W5U
General Description:
Vibegron, identified by CAS number 1190389-15-1, is a notable compound with significant therapeutic applications. Vibegron is a potent, selective beta-3 adrenergic receptor (β3) agonist that relaxes the detrusor smooth muscle of the bladder, thereby increasing bladder capacity. Vibegron was first approved in Japan in September 2018 for the treatment of overactive bladder, a condition associated with distressing symptoms of urge urinary incontinence, urgency, and urinary frequency, and reduced quality of life of patients. On December 23, 2020, vibegron was approved for the same indication in adults. It is available as oral tablets under the market name GEMTESA. Vibegron is the second beta-3 adrenergic agonist approved for the treatment of overactive bladder following , which was approved in 2012. Unlike mirabegron, vibegron is less likely to be associated with drug-drug interactions involving the CYP3A4, 2D6, or 2C9 enzymes.
Indications:
This drug is primarily indicated for: Vibegron is indicated for the treatment of overactive bladder (OAB) with symptoms of urge urinary incontinence, urgency, and urinary frequency in adults. Its use in specific medical scenarios underscores its importance in the therapeutic landscape.
Metabolism:
Vibegron undergoes metabolic processing primarily in: In vitro, CYP3A4 is the main enzyme responsible for the metabolism of vibegron, which plays a minor role in the elimination of vibegron. Two predominant metabolic pathways are oxidation and glucuronidation to form two oxidative metabolites and three glucuronide metabolites. Metabolites have not been fully characterized. This metabolic pathway ensures efficient processing of the drug, helping to minimize potential toxicity and side effects.
Absorption:
The absorption characteristics of Vibegron are crucial for its therapeutic efficacy: The mean Tmax is 1-3 hours. Steady-state concentrations are achieved within 7 days of once-daily dosing. The drug's ability to rapidly penetrate into cells ensures quick onset of action.
Half-life:
The half-life of Vibegron is an important consideration for its dosing schedule: The terminal plasma half-life ranges from 60 to 70 hours. The effective half-life is 30.8 hours. This determines the duration of action and helps in formulating effective dosing regimens.
Protein Binding:
Vibegron exhibits a strong affinity for binding with plasma proteins: Vibegron is 49.6–51.3% bound to human plasma proteins. This property plays a key role in the drug's pharmacokinetics and distribution within the body.
Route of Elimination:
The elimination of Vibegron from the body primarily occurs through: In a radiolabeled drug study, approximately 59% of the radiolabeled dose was recovered in feces, in which 54% of that amount was in the unchanged parent drug form. About 20% of the radioactivity was recovered in urine, in which 19% of the amount was in the unchanged form. Understanding this pathway is essential for assessing potential drug accumulation and toxicity risks.
Volume of Distribution:
Vibegron is distributed throughout the body with a volume of distribution of: The mean apparent volume of distribution is 6304 L. The average blood-to-plasma concentration ratio is 0.9. According to tissue distribution studies in animals, vibegron does not penetrate the blood-brain barrier, suggesting limited potential for CNS toxicity in humans. This metric indicates how extensively the drug permeates into body tissues.
Clearance:
The clearance rate of Vibegron is a critical factor in determining its safe and effective dosage: There is limited information on the clearance rate of vibegron. It reflects the efficiency with which the drug is removed from the systemic circulation.
Pharmacodynamics:
Vibegron exerts its therapeutic effects through: Vibegron selectivity for beta-3 adrenergic receptors is >9000 times higher than for β1AR or β2AR. Vibegron improves clinical symptoms of overactive bladder by increasing bladder capacity without affecting bladder contraction. It significantly increases the functional bladder volume in a dose-dependent manner, which results in prolongation of the interval between voids. In clinical studies, vibegron inhibited detrusor bladder contractions in a concentration-dependent manner, reduced voiding pressure, and increased bladder compliance. In Japanese clinical studies comprising patients with overactive bladder, vibegron significantly improved the frequency of micturition, urgency, and urgency incontinence episodes. The drug's ability to modulate various physiological processes underscores its efficacy in treating specific conditions.
Mechanism of Action:
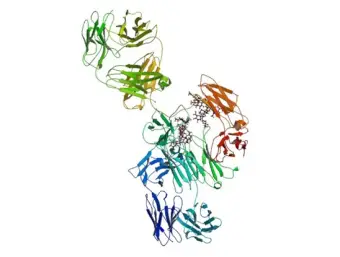
Vibegron functions by: Overactive bladder is characterized by symptoms of urge urinary incontinence, urgency, and urinary frequency. Bladder filling and emptying are regulated by the coordinated communication between sympathetic and parasympathetic systems. Bladder filling occurs via parasympathetic inhibition and the sympathetic hypogastric nerve releasing norepinephrine, which acts on beta-adrenergic receptors responsible for mediating detrusor muscle relaxation. Symptoms of overactive bladder are thought to be caused by the deterioration of the sensory connections between the bladder, spinal cord and brain, leading to changes in the lower urinary tract and abnormal bladder sensations of the urge to void at small bladder volumes. Beta-3 adrenergic receptors (β3ARs) are expressed in the kidneys and lower urinary tract, including ureters, urethra, prostate, and bladder. Vibegron is a selective agonist at β3AR. One vibegron binds to the receptor, β3AR is stimulated and undergoes a conformation change and activates adenylyl cyclases (AC), which promotes the formation of cyclic adenosine monophosphate (cAMP). Increased intracellular cAMP concentration leads to the activation of cAMP-dependent protein kinase A (PKA), which subsequently phosphorylates myosin light chains that are responsible for inhibiting the interaction of actin with myosin dependent on calcium – calmodulin complex. In clinical trials, vibegron increased cAMP levels in a dose-proportional manner. There is evidence that β3AR agonists may also work via sensory mechanisms without directly affecting detrusor muscle motor function. This mechanism highlights the drug's role in inhibiting or promoting specific biological pathways, contributing to its therapeutic effects.
Toxicity:
Categories:
Vibegron is categorized under the following therapeutic classes: Adrenergic Agonists, Adrenergic beta-3 Receptor Agonists, Adrenergic beta-Agonists, Cytochrome P-450 CYP3A Substrates, Cytochrome P-450 CYP3A4 Substrates, Cytochrome P-450 Substrates, Drugs for Urinary Frequency and Incontinence, Genitourinary Smooth Muscle Relaxants, P-glycoprotein substrates, Pyrimidines, Selective Beta 3-adrenergic Agonists. These classifications highlight the drug's diverse therapeutic applications and its importance in treating various conditions.
Vibegron is a type of Antimetabolites
Antimetabolites are a prominent category of pharmaceutical active pharmaceutical ingredients (APIs) utilized in the treatment of various diseases, particularly cancer. These compounds are structurally similar to naturally occurring metabolites essential for cellular processes such as DNA and RNA synthesis. By mimicking these metabolites, antimetabolites interfere with the normal functioning of cellular pathways, leading to inhibition of cancer cell growth and proliferation.
One of the widely used antimetabolites is methotrexate, a folic acid antagonist that inhibits the enzyme dihydrofolate reductase, disrupting the production of DNA and RNA. This disruption impedes the growth of rapidly dividing cancer cells. Another common antimetabolite is 5-fluorouracil (5-FU), which inhibits the enzyme thymidylate synthase, thereby interfering with DNA synthesis and inhibiting cancer cell proliferation.
Antimetabolites can be classified into several subcategories based on their mechanism of action and chemical structure. These include purine and pyrimidine analogs, folic acid antagonists, and pyrimidine synthesis inhibitors. Examples of antimetabolites in these subcategories include azathioprine, cytarabine, and gemcitabine.
Despite their effectiveness, antimetabolites can exhibit certain side effects due to their interference with normal cellular processes. These side effects may include gastrointestinal disturbances, myelosuppression (reduced production of blood cells), and hepatotoxicity.
In conclusion, antimetabolites are a vital category of pharmaceutical APIs used in the treatment of various diseases, especially cancer. By mimicking natural metabolites and disrupting crucial cellular processes, these compounds effectively inhibit cancer cell growth and proliferation. However, their usage should be carefully monitored due to potential side effects.
Vibegron manufacturers | traders | suppliers
We have 2 companies offering Vibegron produced in 0 different countries.
Get in contact with the supplier of your choice:
- Apino Pharma Co., Ltd. from China, product country of origin China
- Global Pharma Tek from India, product country of origin India
Let the supplier know whether you are looking for a product with a specific monograph such as EP (Ph. Eur.), USP, JP, BP or another quality. Or, whether you are looking for hydrochloride (HCl), anhydricum, base, micronisatum or a specific purity.
You can use the filters to find high-quality suppliers. For example, you can select GMP, FDA or ISO certified suppliers. Visit our FAQ page or use the chat box in the corner to get more information about Pharmaoffer.