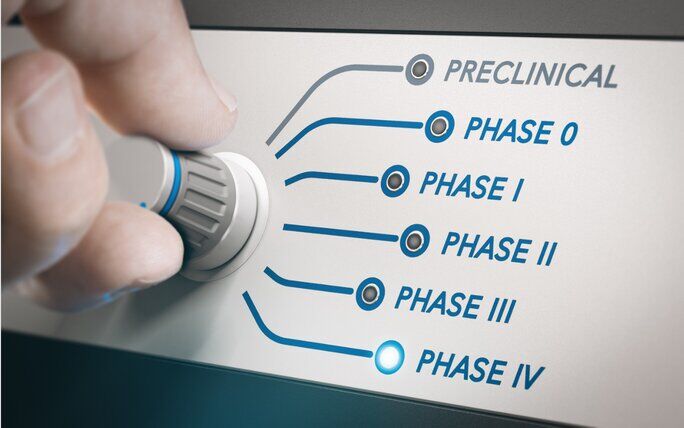
From preclinical trials to post marketing surveillance
everything you need to know about API clinical trials

Su Keles | Posted on April 20, 2023
API stands for Active Pharmaceutical Ingredient, which is the primary component responsible for the healing effect in a drug. An API clinical trial is a series of tests conducted to evaluate the safety and efficacy of a new or existing API.
The tests can be severe and rigorous, as it should, since it affects the well-being and health of the public. The most difficult stage is the first one, the preclinical stage. A study reports that the success rate of each drug discovery stage in was 31.8% for preclinical, 75.1% for phase I, 50.0% for phase II, 58.6% for phase III. Actually, the transition from preclinical stages to human trials is so risky that it is frequently referred to as the “Valley of Death.”
For any pharmaceutical company or academic institution, it is a big achievement to advance a drug candidate to phase I clinical trial after drug candidates are strictly optimized at preclinical stage. The rigid system doesn’t end there. Another study shows that after they have entered clinical studies, nine out of ten drug candidates, would fail during the phase I, II, or III of the clinical trial.
If you are interested on how new APIs are discovered, you can read one of our blogs where you will find information about the whole process from A to Z.
The stages of an API clinical trial are as follows:
- Preclinical stage: This stage involves laboratory testing of the API to determine its safety and effectiveness in animals. The goal of this stage is to gather enough information to support the initiation of clinical trials in humans
- Phase 1 clinical trial: This is the first stage of clinical testing in humans. The goal of this phase is to evaluate the safety of the API and to determine the optimal dosage range. Phase 1 trials typically involve a small number of healthy volunteers.
- Phase 2 clinical trial: This stage involves testing the API in a larger group of patients to evaluate its efficacy and further assess its safety. The focus of this phase is to determine the optimal dosage and identify any potential side effects.
- Phase 3 clinical trial: This is the final stage of clinical testing before the drug is approved for marketing. Phase 3 trials are conducted on a larger scale and involve a larger number of patients. The goal of this phase is to confirm the safety and effectiveness of the API, and to compare it to existing treatments or a placebo.
- Post-marketing surveillance: After the drug is approved for marketing, post-marketing surveillance is conducted to monitor the safety and effectiveness of the drug in a larger population. This helps to identify any rare or unexpected side effects that may not have been detected during clinical trials.
Overall, an API clinical trial is a complex process that involves multiple stages of testing to ensure that the drug is safe and effective for use in humans.
We summarized the steps above, but we want to get into more details and have a deep look at each one of the steps. So bear with us, as we dive into the complex and rigorous world of API clinical trials.
Preclinical stage
The preclinical stage of an API clinical trial is the first stage of drug development, and it is conducted before the drug is tested on humans. This stage involves extensive laboratory testing of the API to gather information about its pharmacological properties, safety, and efficacy.
During the preclinical stage, the API is tested in vitro, which means it is tested in laboratory conditions using cell cultures, tissues, or organs. The API is also tested in vivo, which means it is tested in animals to evaluate its safety and efficacy. The preclinical stage aims to provide the necessary information to support the initiation of clinical trials in humans.
The preclinical studies are conducted in compliance with the guidelines and regulations set by the regulatory authorities such as the US Food and Drug Administration (FDA).
The preclinical stage typically involves the following activities:
- In vitro studies: In vitro studies are conducted to evaluate the API’s pharmacological properties, such as its mechanism of action, potency, and selectivity. These studies also help to identify any potential toxicity or adverse effects of the API.
- Animal studies: Animal studies are conducted to evaluate the API’s safety and efficacy in vivo. These studies involve administering the API to animals to evaluate its pharmacokinetics (how the drug is absorbed, distributed, metabolized, and eliminated in the body), pharmacodynamics (how the drug interacts with the body’s physiological systems), and toxicology (how the drug affects the animal’s organs and tissues).
- Formulation development: During the preclinical stage, researchers also develop a formulation of the API, which is the final drug product that will be administered to humans. The formulation is optimized to ensure that the API is stable, safe, and effective when administered to humans.

Phase 1
A Phase 1 clinical trial is the first stage of testing a new API in humans. The goal of a Phase 1 trial is to evaluate the safety of the API and to determine the optimal dosage range.
Phase 1 clinical trials are typically conducted on a small number of healthy volunteers, usually between 20-80 individuals, who are closely monitored by medical professionals. During this phase, the API is administered to the volunteers, and the researchers collect data on its pharmacokinetics, pharmacodynamics, and any adverse effects that may occur.
The primary objectives of a Phase 1 clinical trial are as follows:
- Safety: The primary objective of a Phase 1 trial is to evaluate the safety of the API in humans. The researchers closely monitor the volunteers for any adverse effects, and they adjust the dosage if necessary to ensure that the API is safe for human use.
- Pharmacokinetics: Phase 1 trials also evaluate the pharmacokinetics of the API, which refers to how the drug is absorbed, distributed, metabolized, and eliminated in the body. This information helps to determine the optimal dosage and dosing frequency for subsequent clinical trials.
- Pharmacodynamics: Phase 1 trials also evaluate the pharmacodynamics of the API, which refers to how the drug interacts with the body’s physiological systems. This information helps to determine the therapeutic potential of the API and its mechanism of action.
- Dosage: Phase 1 trials aim to identify the optimal dosage range for the API in humans. This information is used to design subsequent clinical trials and to determine the maximum safe dosage for patients.
- Formulation: Phase 1 trials also evaluate the formulation of the API, which is the final drug product that will be administered to patients. This information is used to optimize the formulation to ensure that it is safe and effective for use in humans.

Phase 2
A Phase 2 clinical trial is the second stage of testing a new API in humans. The goal of a Phase 2 trial is to evaluate the efficacy and further assess the safety of the API in a specific patient population.
Phase 2 clinical trials are typically conducted on a larger number of patients, usually between 100-500 individuals, who have the target disease or condition that the API is intended to treat. During this phase, the API is administered to the patients, and the researchers collect data on its efficacy, safety, and optimal dosage.
The primary objectives of a Phase 2 clinical trial are as follows:
- Efficacy: The main objective of a Phase 2 trial is to evaluate the efficacy of the API in treating the target disease or condition. The researchers measure the API’s effectiveness in achieving the desired therapeutic outcome and compare it to a control group that receives a placebo or standard of care treatment.
- Safety: Phase 2 trials further evaluate the safety of the API in patients. The researchers closely monitor the patients for any adverse effects and determine the maximum safe dosage for patients.
- Dosage: Phase 2 trials aim to identify the optimal dosage range for the API in the specific patient population. This information is used to design subsequent clinical trials and to determine the maximum safe dosage for patients.
- Pharmacokinetics and pharmacodynamics: Phase 2 trials continue to evaluate the pharmacokinetics and pharmacodynamics of the API in the specific patient population. This information helps to determine the optimal dosing regimen and potential interactions with other medications.

Phase 3
A Phase 3 clinical trial is the third and final stage of testing a new API in humans before it can be approved by regulatory agencies for marketing and distribution. The goal of a Phase 3 trial is to confirm the efficacy and safety of the API in a larger patient population.
Phase 3 clinical trials are typically conducted on a much larger number of patients, usually between several hundred to several thousand individuals, who have the target disease or condition that the API is intended to treat. During this phase, the API is administered to the patients, and the researchers collect data on its efficacy, safety, and potential adverse effects.
The phase 3 objectives are similar to the phase 3 objectives, with usually an emphasis on long-term effects. Phase 3 trials may also evaluate the long-term effects of the API in patients. This information helps to assess the potential risks and benefits of the API over an extended period.
Post-marketing surveillance
Finally, we reach the state where the drug is out in the public, and ready to be consumed. But the control and safety procedures do not end here. Have you ever googled the website of a pharmaceutical company? Well, if you do, you can find in most of the websites a “contact us for complaints about a product” button. This is what we call post-marketing surveillance.
Post-marketing surveillance is usually carried out through various methods such as voluntary reporting of adverse events by healthcare professionals and patients, observational studies, and clinical trials. These methods help to identify any safety concerns or efficacy issues that were not detected during the preclinical and clinical trial stages.
Pharmaceutical companies are required to collect and report safety data on the API as part of their post-marketing surveillance obligations. Regulatory agencies such as the FDA use this safety data to monitor the safety and efficacy of the API, and may require additional safety studies or take regulatory action if safety concerns arise.
Conclusion
API clinical trials are a critical component of the drug development process, and they are essential in ensuring that new APIs are safe and effective for use in humans. The five stages of API clinical trials, but mainly the preclinical stage, phase 1, phase 2, and phase 3 trials, help to assess the safety and efficacy of APIs in humans.
The preclinical stage involves laboratory and animal testing to evaluate the safety and effectiveness of the API. Phase 1 trials assess the safety, tolerability, and pharmacokinetics of the API in a small group of healthy volunteers. Phase 2 trials evaluate the efficacy and safety of the API in a larger group of patients with the target disease or condition, and Phase 3 trials confirm the efficacy and safety of the API in a large patient population. After regulatory approval, post-marketing surveillance is conducted to ensure that the API continues to be safe and effective for use in patients.
Thank you for reading!
FAQ
What is an API Clinical Trial?
An API (Active Pharmaceutical Ingredient) clinical trial is a series of tests designed to assess the safety and efficacy of a new or existing API. These trials are essential for ensuring that the API is safe and effective for use in humans.
What is the "Valley of Death" in API clinical trials?
The "Valley of Death" refers to the high-risk transition from preclinical stages to human trials. Advancing a drug candidate to phase I clinical trial is a significant achievement for any pharmaceutical company or academic institution.
Why are API clinical trials critical for drug development?
API clinical trials ensure that new APIs are safe and effective for human use. They involve multiple stages of rigorous testing, from preclinical laboratory tests to large-scale Phase 3 trials, followed by post-marketing surveillance to ensure ongoing safety.





Check out all other blogs here!